Given the special features of the design and surface of implants, combined treatment including mechanical and chemical therapies is essential.
Below are some suggested treatment protocols, although you must keep in mind that they have limitations, as there are very few quality clinical studies validating them. Existing therapy regimes proposed by different authors until now for managing peri-implant diseases are based on the evidence available for the treatment of periodontitis.
Treatment of Peri-implant Mucositis:
Given that peri-implant mucositis and peri-implantitis are associated with the development of biofilm on the implant surface, treatment has been proposed with the aim of reducing bacterial load, which would lead to the eradication of the infection. The different modes of therapy include mechanical treatment with carbon fibre curettes, plastic curettes, titanium curettes or specially designed ultrasonic tips, submucosal released antimicrobials, systemic antimicrobials, laser or a combination of the previously mentioned methods. Very few studies have assessed these types of treatments, although it can be concluded that: Non-surgical mechanical therapy as a sole method, does not seem to be effective in treating peri-implant mucositis.
Treatment of Peri-implantitis:
The ideal therapy for peri-implantitis must include several aspects:
- Removal of peri-implant submucosal biofilm. The treatment of peri-implantitis must be aimed at reducing/removing the pathogens that cause the disease (anaerobes).
- Implant surface decontamination and conditioning.
- Reduction/removal of the sites that cannot be kept free of plaque using oral hygiene methods. Promote the establishment of a more aerobic environment (reducing peri-implant pocket) to avoid the establishment of submucosal microbiota.
- Establishing an efficient plaque control regime to prevent mucositis and re-infection of residual pockets.
- Filling of bone defects
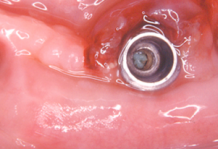
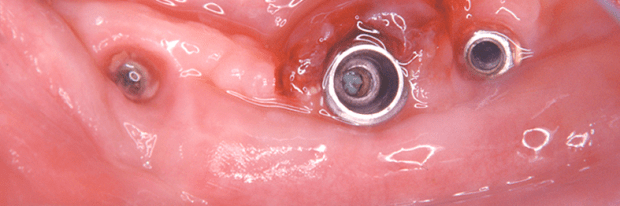
Surface decontamination:
After surgical exposure of the contaminated implant surface, different measures have been used including mechanical, chemical, photodynamic or a combination of these with the goal of eradicating the infection, reversing inflammation and providing a surface favourable for possible bone regeneration and re-osseointegration. Various methods have been used without achieving a definitive gold standard. For example, air jet abrasion, saline flush, citric acid treatment, laser therapy, peroxide treatment, ultrasonic and manual debridement and topical application of various drugs. The various options have been associated with some advantages and disadvantages, such as damage to the implant surface with mechanical or laser therapy, and the failure to remove all potentially harmful cellular components when using chemical treatment only.
Despite obtaining different results, all studies have proven that all surface debridement methods are able to solve the inflammatory lesion, but fail to obtain significant re-osseointegration along the surface of the previously contaminated implant. Histological studies show the formation of a connective tissue capsule separating the implant surface from the adjacent bone in the majority of cases, except for in the most apical portion of the lesion.
Metal curettes and ultrasonic tips cause damage to the titanium implant surface. Abrasive air jet systems avoid this surface damage but can cause surgical emphysema. Delmopinol forms a film on the titanium surfaces which may interfere with the potential re-osseointegration. The formation of this film is enhanced on rougher implant surfaces.
In short, peri-implantitis can be solved by different surface decontamination methods. However, there is evidence indicating that open debridement along with surface decontamination does not obtain significant re-osseointegration even though new bone is regenerated in some of the defects.
Regenerative treatment:
Diverse regenerative methods have been used with autologous bone, allo- and xenografts and resorbable and non-resorbable membranes. In general, best results have been found with these procedures when compared to open debridement and bacterial decontamination as the sole treatment. Although, the variability in the results does not allow us to describe an optimal treatment protocol. This variability may be due to inconsistencies in morphology and size of defects.
Generally, the use of membranes alone or grafting material alone, result in more bone filling than debridement as a sole treatment. In relation to re-osseointegration, the sole use of membranes and grafting alone yielded better results than open debridement. The best results in bone filling and re-osseointegration were found when membranes were combined with grafting material.
More quality studies are needed to help clarify these issues.
Use of antiseptics in the treatment of peri-implant diseases
The use of coadjuvants such as 0.12% Chlorhexidine mouthrinse or gel is effective in controlling and reducing the oral biofilm that causes peri-implant mucositis and peri-implantitis.
Currently numerous scientific studies exist in the literature that support chlorhexidine as the best topical use antiseptic agent, although not all formulations containing chlorhexidine ensure the same effectiveness.
It is very important to study the different components of a formula to avoid possible interactions, and to study its pharmaceutical formulation. Pharmaceutical formulations adding cetylpyridinium chloride to chlorhexidine have proven to obtain the best results. The combination of these two active substances achieves maximum control of the microbial load responsible for peri-implant diseases.
 initiative
initiative