The data reflects the importance of biofilms as a source for local infections that can trigger complications on a systemic level.
Many non-pathogenic organisms exist that produce biofilms and do not cause disease. Some even play a protective role, such as lactobacilli present in the vagina, whose biofilm maintains an acidic vaginal pH, preventing the colonisation and growth of pathogenic microorganisms, such as Gardnerella vaginalis.
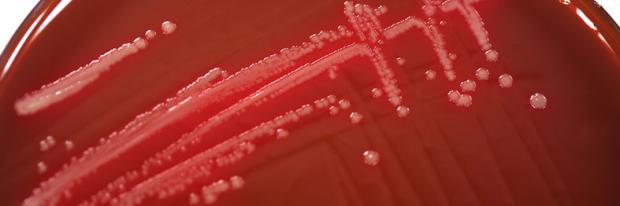
In contrast, epidemiological studies have found evidence linking biofilm with infectious processes with common characteristics: presence of adherent, biofilm-producing bacteria, infections induced by small bacterial innoculants, bacterial biofilm-mediated resistance to host defense mechanisms and to antimicrobial treatment, infections commonly caused by Staphylococcus aureus, Staphylococcus epidermidis and Pseudomonas aeruginosa, the presence of inflammation, damaged cell tissue and necrosis of the tissue-implant interface (Gristina et al., 1994)1.
Statistics show the importance of biofilms as a source of infection. According to a 2008 report, 1.7 million infectious processes were reported with 99,000 deaths per year in the United States and 3 million infections with 50,000 deaths per year in the European Union (Perencevick et al., 2003)2, with nosocomial infections caused by biofilm-infected medical devices being one of the main sources (urinary tract [32%], pneumonia [15%], septicaemia [14%] and other locations [22%]) and higher costs for public health (Castrillón-Rivera et al., 2010)3.
Chronic infectious diseases caused by biofilm-forming bacteria, are of medical interest because they rarely respond to antibiotic treatment and cannot be prevented through immunisation. Some diseases that have been proven to be directly associated with infections from biofilms include: caries, gingivitis, periodontitis, valvular endocarditis, otitis media, chronic microbial prostatitis, cystitis, cystic fibrosis and septicaemia. The main microorganisms associated with these infections are Pseudomonas aeruginosa, Staphylococcus epidermidis, Streptococcus aureus, gram-positive cocci, gram-negative anaerobic bacteria and some fungal species from the Candida and Aspergillus genera (Lasa et al., 1995)4.
Gram-positive bacteria that most commonly colonise medical devices (venous catheters, connectors, endotracheal tubes, intrauterine devices, prosthetic heart valves, pacemakers, dialysis catheters, urinary catheters, hip or knee prostheses, laryngeal, prostheses etc.) are Enterococcus faecalis, Staphylococcus aureus, Staphylococcus epidermidis and Streptococcus viridans; and, among the gram-negative ones, Escherichia coli, Klebsiella neumoniae, Proteus mirabilis and Pseudomonas aeruginosa. These microorganisms come from the skin of patients, from their caregivers, from the water or environment and irreversibly adhere to the submerged surfaces of the devices, where extracellular polymers form and biofilms are produced. Several different methods to control the emergence of biofilms on catheters and other devices have been used, including aseptic techniques during implantation, the application of topical antibiotics, reduced implant time, use of filters in intravenous lines, lumen coating with antimicrobial or anticoagulant agents and extraction of contaminated implants, among others (Castrillón Rivera et al., 2010)3.
Detachment of cells or cell aggregates and infective dose
Biofilm development is a dynamic process of growth and separation (detachment) of bacterial cells and aggregates that can disperse and colonise new surfaces or new hosts (through inhalation, ingestion or erosion). This dispersion process of isolated microcolonies with antibiotic resistance phenotype, results in the production of chronic bacterial infections. The detachment of these microcolonies can also cause high risk for the formation of emboli, which, in turn may have clinically severe implications including stroke or pulmonary events, if they reach the capillary bed.
The formation of biofilms by certain pathogenic species seems to facilitate the survival of these in the environment and in the host. This could be due to the accumulation and dispersion of a sufficient number of pathogens to constitute an infective dose – the minimum amount of microorgansms able to cause infection. Furthermore, the heterogeneous microenvironments that can be found within biofilms may promote a differentiated population of microorganisms with phenotypic and genotypic variants that ensure survival to changing environmental conditions, which would also promote infection (Costerton et al., 1994)5.
Endotoxin production
Some gram-negative bacterial species found in biofilms on medical devices produce endotoxins which, in turn, can cause an immune response in the patient. Various studies have shown a correlation between the number of bacteria within biofilms and the endotoxin concentration (Vincent et al., 1989)6, although none has been able to determine the concentration and kinetics of endotoxins released from biofilms.
Resistance to the host immune system
In vitro studies have shown that biofilms where the S. epidermidis bacterial species is found interfere with the phagocytic activity of microphages (Shiau and Wu, 1998)7.
It has been observed that bacteria can transfer plasmids during conjugation within biofilms, and that these plasmids can carry antimicrobial resistance factors. The physical proximity of the cells within biofilm microcolonies facilitates conjugation, compared to the same process in planktonic organisms (Ehlers and Bouwer, 1999)8. This may be particularly relevant in the case of biofilms on permanent medical devices, where antimicrobial-resistant organisms could be spread from one patient to another via the hands of healthcare personnel.
Ecological Plaque Hypothesis
The oral cavity is protected against the colonisation by exogenous pathogens by a beneficial biofilm made up of some 20-30 different bacterial species, including Streptococci and Actinomyces spp. (Lasa, 2005)4.
Bacterial plaque can be acidic or basic in nature, depending on the type of dominant bacteria that are found within. Acidogenic plaque is dominated by bacteria that produce acids when metabolising sugars from diet (such as Streptococcus mutans and Lactobacillus acidophilus); lactic acid, the final product of this metabolism, pours over tooth surfaces, causing a destructive tooth process (caries). Basogenic plaque is dominated by bacteria that produce basic substances (Porphyromonas gingivalis, Treponema denticola, Treponema socranskii, Veillonella spp, Capnocytophaga spp, Actinomyces spp, Aggregatibacter actinomycetemcomitans) which cause inflammation and subsequent periodontal destruction (periodontal disease).
Acidogenic plaque
Bacteria that produce acids through metabolism
Initiate the tooth destruction process, causing Caries.
Basogenic plaque
Bacteria that produce basic substances
Cause inflammation and subsequent periodontal destruction, in other words, Gingivitis and Periodontitis.
In dental plaque, or oral biofilm, bacteria live together in equilibrium while external conditions are maintained constant. This equilibrium may be altered by the intake of food or drink that are rich in sugars, favouring the development of bacterial species that ferment sugars, creating an imbalance in the bacterial population and leading to the development of acid-producing species.
Marsh and Martin (2000)9 use the ecological plaque hypothesis to explain the aetiology of periodontal disease. This hypothesis suggests that the changes in local environmental conditions in the subgingival region, such as an increase in crevicular fluid during inflammation, favours the growth of strict anaerobic proteolytic species, predisposing the gingival area to disease. For these authors, it is still unclear whether or not gingivitis is a necessary stage for the development of different types of periodontitis or if this may appear independently. Nevertheless, certain bacterial species that dominate in periodontitis, which are not detected in periodontally healthy individuals, have been found at a low percentage in gingivitis. This situation suggests that the conditions developed during gingivitis, such as bleeding and suppuration, may promote the growth of species involved in periodontitis.
- Gristina AG. Biofilms and chronic bacterial infections. Clin Microbiol Newsletter 1994; 16: 171-178.
- Perencevich EN, Sands KE, Cosgrove SE, Guadagnoli E, Meara E, et al. (2003) Health and economic impact of surgical site infections diagnosed after hospital discharge. Emerg Infect Dis 9: 196–203. abdoi: 10.3201/eid0902.020232
- Castrillón-Rivera LE, Palma-Ramos A, Padilla-Desgarennes MC. Importancia de las biopelículas en la práctica médica. Dermatol Rev Mex 2010;54(1):14-24.
- Lasa I, del Pozo JL, Penadés JR, Leiva J. Biofilms bacterianos e infección. Anales Sis San Navarra, 2005, (28)2
- Costerton JW. Biofilms, the customized microniche. J Bacteriology 1994;176:2137-42.
- Vincent, F. C., A. R. Tibi, and J. C. Darbord. 1989. A bacterial biofilm in a hemodialysis system. Assessment of disinfection and crossing of endotoxin. ASAIO Trans. 35:310–313.
- Shiau, A.-L., and C.-L. Wu. 1998. The inhibitory effect of Staphylococcus epidermidis slime on the phagocytosis of murine peritoneal macrophages is interferon-independent. Microbiol. Immunol. 42:33–40.
- Ehlers, L. J., and E. J. Bouwer. 1999. RP4 plasmid transfer among species of Pseudomonas in a biofilm reactor. Water Sci. Technol. 7:163–171.
- Marsh, P.; Martin, M.2000: Oral Microbiology. Fourth edition. Wright. England.
 initiative
initiative